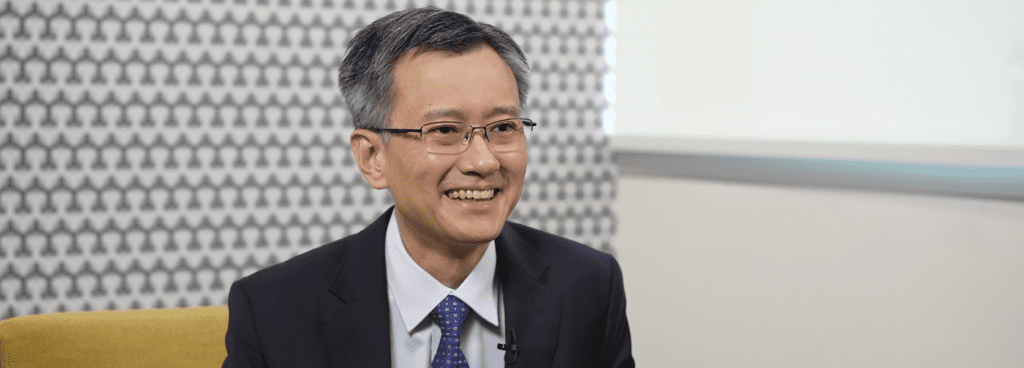
Sign up for the Master Pack to unlock exclusive contents on STRONG-HF, including STRONG-HF primary outcomes infographic and exclusive interviews with Prof Mebazaa and APAC KOLs.
Congestion remains in many AHF patients at discharge
The topic we heard since the beginning of the session is about heart failure and about congestion. We need more close collaboration between Asia and Europe to try to confirm the results that come from the ESC database that were analyzed by Heart Failure Association, showing that 70 percent of the patients were congestive at admission. But more importantly, and this is probably true anywhere in the world, when we say to the patient “Bye Bye” by signing the report and saying that everything is fine, very likely, at least 30 percent of those patients are still congested when they go back home.
Pre and post-discharge management of AHF patients
The topic then is how are we going to avoid readmission because every failure patient that is readmitted is really sad, feels anxiety and it’s really a major worsening in quality of life. When you come back to the ESC but also to the North American guidelines, it was written just a sentence saying, please see your patient back within one to two weeks without necessarily saying what we should do when we see this visit.
There is a paradox in heart failure. There is a big part of paradox in heart failure. Heart failure is killing today, much more than any cancer. Heart failure is killing much more than any cancer both in males and females. In this paradox we have treatment to cure heart failure, at least to prevent and we heard that many times but many of the speakers to prevent re-admission and those are the four therapies that were mentioned several times. Then heart failure is killing more than cancer. We have the chemotherapy to treat heart failure.
Major gaps in GDMT among eligible patients
However, we are not using the drugs to cure heart failure, and we know that all around the world and probably there is no exception. The four drugs are used less than 25 percent of the time. And whether the chemotherapy was complete if we give the full dose of chemotherapy for heart failure, and then only one to two percent of the patients would be adequately treated.
STRONG-HF
STRONG-HF surprisingly came here in Asia and it came from this study here where you can recognize co-authors from many Asian countries. And in fact we showed a large cohort of 20 thousand acute heart failure patients from both Europe and Asia, different countries in Asia. We follow them for one year after acute heart failure episodes. It shows that when beta blocker and RASi were given combined in patients, their survival was much better than patients who didn’t have anything.
Primary endpoint
Immediately, this is the results of STRONG. You see exactly the same result. In fact, we just repeated what we did many years ago. Here with many Asian countries. Here prospectively, we gave beta blocker, RASi, and MRA at the high full dose and we could repeat exactly the same results and improvement in heart failure readmission and death.
Study design
How did we do this? The design was rather easy. Patients were going to be discharged from acute heart failure in one arm. Patients were followed by the cardiologists in town and in the other arm we gave before discharge. This is very important. Before discharge, we gave half of the optimal dose of beta blocker. Plus, at the same minute, half of the optimal dose of RASi and half of the optimal dose of MRA. One week later, we were asking the patient to come back to check that combining the three drugs was safe and I will show you in a minute how we did it. At week two, we ask the cardiologists regardless of anything else to push the three medications to full dose except if there is any safety issue. I will come back in a minute to tell you what kind of safety issue. And then the patients were followed for the next weeks and the primary endpoint was 180 days.
Universal assessment of congestion
What did we do in the visit? The guidelines both in the US and Europe were saying, you need to see the patients, but they didn’t say what to do during the visit. And in fact, we had a very strict procedure in STRONG. We asked every physician to do the clinical signs: fatigue, dyspnoea, oedema, body weight, heart rate, blood pressure and we asked to have at every visit by biology. Natriuretic peptides that was a main player but also potassium, creatinine very important and hematocrite.
NT-proBNP can be used to monitor patients for GDMT uptitration
You will see that we didn’t do any rocket science in STRONG. We did exactly what you are doing in your practice but we put them all together. We said if NT-proBNP is going to increase more than when patients were discharged, you uptitrate loop diuretics, green light. If NT-proBNP goes down, then you stop uptitration. For beta blocker, if NT-proBNP goes down, heart rate is fine, systolic blood pressure is fine, you uptitrate to full dose at week two and it is also the same for ACEi. However, in very few cases, when we saw NT-proBNP going up, there is radical hypertension, and then we would stop uptitration and this is exactly what we did here.
And in most of the cases we had the NT-proBNP was stable, patient was admitted, here the blue box is the hospital. Before discharge, you see that the NT-proBNP in green was going down and then we were giving half of the dose of the three drugs. In week two, NT-proBNP was still coming down. This was the majority and then we gave full dose of GDMT. In few cases, NT-proBNP after discharge and after combining the three medications at half dose, NT-proBNP was going up. Then we asked the investigator and we ask you, if you follow the STRONG procedure. If you see NT-proBNP going up, it’s very easy. We said it earlier. You just increase the dose of diuretics to decongest the patient. You wait for one to two weeks. You see NT-proBNP going down and then you just go to full dose of all the medications. We succeeded to have half of the patients with full dose of beta blocker and full dose of RASi and even 80 percent of the patients who had a full dose of MRA.
Improvement in congestion
This is one of the incredible results with STRONG. Oral medications, combining the three oral medications, despite a lower diuretics dose compared to usual care, achieved an incredible congestion. And you can see here all the parameters who would dream to see improving, they were improved, just because we gave the full medications primary endpoint as I showed earlier was positive, quality of life was also improved, and the mortality was numerically better and all those parameters were much more improved, differences much greater if we remove the patients who died from Covid.
First post-discharge therapy of HFpEF
A question that I often have since this paper came out and the beautiful paper of Matteo Pagnesi that came out a few weeks ago, does it work in HFpEF? This was the big positive surprise in STRONG. The results work a little bit better and indeed it works as well in low ejection fraction and preserved ejection fraction. But here we have the feeling that it’s even better with patients with preserved ejection fraction and Matteo showed here in the x-axis, you see all the baseline left ventricular ejection fraction. And you see that the positive effect of STRONG is true regardless and this is very good, why? Because we just heard that a minute ago by Professor Rozano. The medications for HFpEF just came out. We just had a new recommendation on HFpEF and here was STRONG for the first time we say when there is an acute decompensation and patient with HFpEF we have a solution. For years myself, I was crying to ask the patient to go back home without any medication because they were having a decompensation for HFpEF. And here for the first time at least for the first six months, we can give them therapy and it can improve.
Another question that I often have is age. As you can see here, there is no difference in age. The positive results of STRONG is true.
This is the paper of Mattia Arrigo in the European Journal of Heart Failure. Indeed, we had a slightly higher adverse event but no difference in serious adverse event or fatal serious adverse event. In STRONG when we started the study, only beta blocker, ARNi, RASi and MRA were indicated then we pushed to have those three medications fully giving to the patients within two weeks after discharge. Indeed in the meanwhile, glyphosyn came out. The study with empulse with positive results. It’s very likely if you had to redo it indeed, you would have done the four and very likely the results would be as good and probably, even better than STRONG now has to be seen with the four medications.
Review on the management of AHF patients
This is the first time I show this figure of a review that will come out in few weeks during the ESC meeting in Amsterdam. Together with a meeting, you will see a great review on acute heart failure that is published in Europe Heart Journal. With this figure where we show at admission with acute heart failure, how we should treat the first day. Here you have a patient at discharge and you see here in white, the oral heart made fairly medications that should be started by half before being discharged and we should not forget to see the patient again examining congestion. Looking what we are doing by giving a full therapy is safe, including biological exam and clinical exam. And if everything goes very well, you can climb the mountain, probably Fujiyama, but not so much in Singapore.