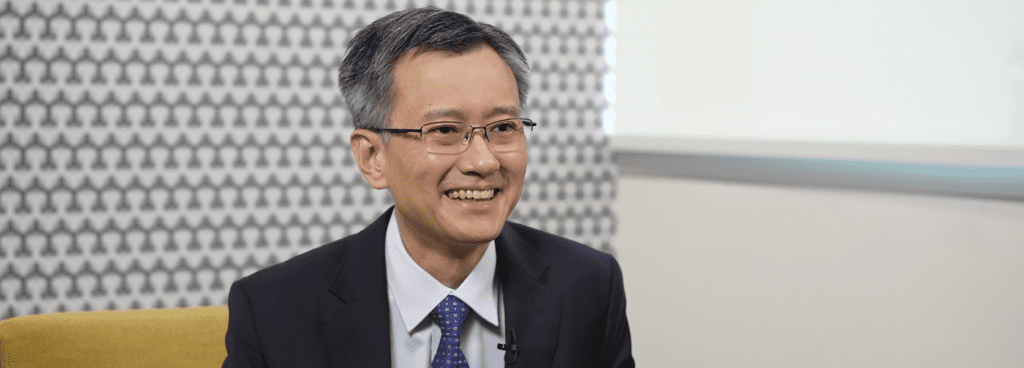
Why is it important to actively screen for PMI/MINS after NCS?
First, we should know what is PMI. PMI stand for perioperative myocardial infarction or injury. Causes of PMI can be cardiac or non-cardiac in origin, in the end approximately 70% are type 2 MI. Having PMI means you have about 10% higher chance of dying at one year. I mean the absolute risk difference.
Data from BASEL-PMI study showed that one in six of the intermediate to high risks patients undergoing intermediate to high risk non cardiac surgery would have PMI. From that number, only 20% had signs or symptoms of ischemic event, and only 6% had typical chest pain. Without PMI screening, we won’t know anything and we just discharge them, and they get the CV event after that, some may not survive. This is the reason why we should set an active screening system to ensure that we won’t miss PMI in our patients.
What is the current practice to screen patients for high risk of CVD/MI after NCS and what is the value of hs-cTn as a screening tool?
We have been using Revised Cardiac Risk Index for more than 15 years. The last perioperative guideline we are using went back to 2014, the ACC/AHA guideline. Having read the 2022 ESC guidelines makes me feel that now we have something more accurate and more objective than a previous clinical risk score. Perioperative cardiac troponin is truly a paradigm shift in perioperative management in NCS. Now with just a few cardiac troponin tests, we can get information on pre-operative risk, peri-operative cardiac event, or even the risk of post operative long-term mortality. Cardiac troponin has become such a valuable tool as a screening test in NCS.
How should the current Guideline Recommendations be implemented?
Like many guidelines, that provide us the best up-to-date evidence, produced from a higher standard medical care. Some suggestions may not be practical to do in a local practice. So my thought would be we try to start the program first, to see how it goes. Then we collect the data, such as prevalence of PMI and the mortality associated with it, so we know the magnitude of the problem. A local care plan for patients with PMI can be made, using the flow diagram in the guideline as a guidance. I’ve seen some hospitals use this strategy, and it works.
Which patient profile would be most suitable for troponin measurement?
In the new guidelines, it said that patients who are older than 65 years old, who have ASCVD, and anyone who carry co-morbidities, undergoing intermediate to high-risk surgery are entitled for the screening test. But if you think that you cannot afford in terms of budget and workforce or healthcare resources, you can just increase the threshold by choosing those who are at a higher risk first.
How many times should troponin be measured and what should be the cut-off values?
It’s three times for me, before NCS pre-operative, day 1 and day 2 after NCS. The given cut off value of 14ng/L, at this moment, I’m happy to use it.
What are the potential barriers for implementation?
I think the awareness of PMI is the key. Since the awareness is very low, gathering multidisciplinary team to work together to implement it in daily clinical practice and the changing of the misperception of higher work load is not easy to overcome. Some say about reimbursement issues, which I do see as a potential problem in some countries as well.
What should be the in-house management after PMI detection (especially consultation criteria)?
As per each institution, there should be a local patient care pathway specific to the etiology of PMI, as recommended by 2022 ESC guidelines framework.
Active alignment across multi-disciplinary specialties is highly encouraged to ensure efficiency of the utilization of available resources in each institution. This would enable seamless clinical implementation for the best patient outcomes to diagnose silent AMI in the perioperative phase.