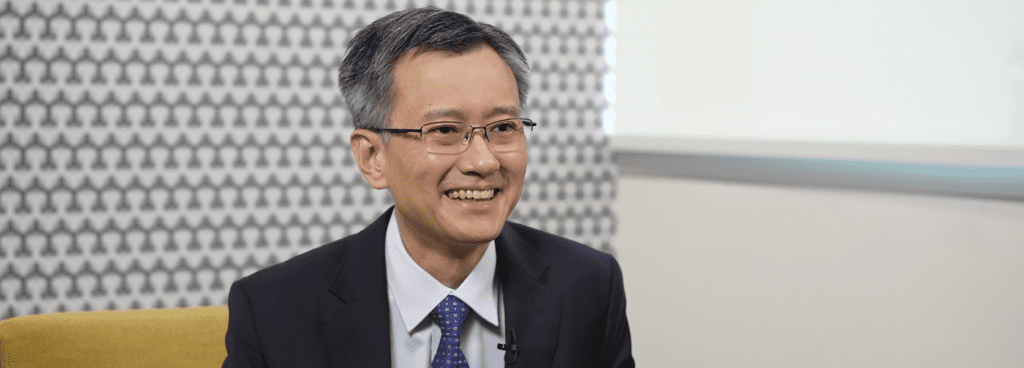
Q1 What are the current challenges in heart failure for patients in Hong Kong?
Similar to other parts of the world, heart failure is prevalent in Hong Kong affecting around 1-2% of the population, which means more than 70 thousand patients will suffer from heart failure in Hong Kong. Heart failure also carries high mortality with more than 50% of the patients die at 5 years after being diagnosed to have heart failure according to our local study. In addition, heart failure imposed significant burden to our healthcare service with more than 20,000 hospitalization related to heart failure each year. Although nowadays we have many evidence-based treatments to improve morbidity and mortality of heart failure as well as comprehensive international guidelines for us to follow, our local study revealed that the uptake of these well-proven heart failure therapies in real world was disappointing. Furthermore, in a public survey carried out by our society few months ago, we found that most Hong Kong citizens don’t understand what is heart failure, what are the common heart failure symptoms, and how severe is the disease. We believe the difficulties to provide heart failure service in a real world setting and the low public awareness are the major challenges in heart failure management in Hong Kong.
Q2 Why is the Hong Kong Heart Failure Society form and what does it aim to achieve?
In response to the challenges in heart failure management in Hong Kong, a group of colleagues who shared the similar vision met together and we all agreed that given the high prevalence of the disease, it would never work if we work in an individual manner. As a result, a heart failure network was initially formed in 2018 for better communication, case and experience sharing and heart failure service coordination. As time goes by, the group on one hand recognised the need to work more to address the unmet need for heart failure management in Hong Kong. On the other hand we received many valuable advice from our distinguished international advisers that a society dedicated to heart failure should be formed so that colleagues can join together to fight the war such as the case of Heart Failure Society of America, British Society of Heart Failure and Heart Failure Society of Singapore. Therefore, the Hong Kong Heart Failure Society was formed last year with an aim to improve professional education, to raise public awareness, to enhance heart failure service, and finally through all these aim to achieve better quality of life and longevity for heart failure patients in Hong Kong.
Q3 What are some key initiatives the Hong Kong Heart Failure Society seeks to implement in the near future
Our society will implement initiatives in 3 main areas, first public awareness, second professional education, and third service enhancement. To arouse public awareness, we are going to publish a heart failure information booklet incorporating QR code linked to short video clips to provide key information related to heart failure. We will also setup social media pages, participate in TV and radio interviews as well as write newspaper articles to disseminate health information to the public. For professional education, we are going to hold webinars on different cutting-edge clinical topics, organise workshops for echocardiogram and mechanical circulatory support device, and hold a cardiomyopathy symposium to recognise the challenges in managing specific form of cardiomyopathies. Additionally, we will organise an end-stage heart failure forum to celebrate the 30th anniversary of heart transplant service in Hong Kong as well as to promote the importance of guideline directed medical therapy to delay the progression to end stage heart failure. Lastly, we will try to identify the major service gap for heart failure management in Hong Kong and advise the administrative on different possible ways to improve the service.
Q4 How can the Hong Kong healthcare ecosystem better manage heart failure patients?
Although nowadays heart failure management are quite standard with good international guidelines for us to follow. It is not always easy to carry out those guideline recommendations in a real world settings. For example, for patients admitted to hospital with symptoms and signs compatible with heart failure, echocardiogram should be a reasonable next step assessment to identify any structural lesions such as valvular heart disease as well as to delineate the ejection fraction, which would have important implication on management strategies. However, in real world setting, waiting time of echocardiogram is commonly in terms of months if not years in public system in Hong Kong. In addition, biomarkers for heart failure, which received class I recommendation in heart failure guidelines, are not available in most of the public hospital in Hong Kong. These critical steps in heart failure evaluation should be adequately addressed, otherwise it will cause significant bottleneck effect in implementing appropriate heart failure treatments. For patients discharged from hospital after acute decompensated heart failure, early post-discharge period is the most vulnerable period of decompensation and re-hospitalization. Currently, it is not uncommon to have out-patient follow up, up to four to six months after discharge and patients might have decompensation again presented to emergency department before follow-up. Therefore, timely transitional care and multidisciplinary heart failure service are crucial and should be developed to reduce the risk during this most vulnerable period. For out-patients who found to have suspected heart failure by primary care, currently the usual waiting time for new case cardiology out-patient clinic appointment is in terms of months to years and designated heart failure clinic was not available in most public hospitals in Hong Kong. Therefore, the development of heart failure clinic service would be useful to provide timely assessment and management for patients suspected to have heart failure by primary care.
Q5 What are some of the cross-country collaborations within APAC and what to they aim to accomplish?
I think we all shared similar vision to tackle heart failure as a major healthcare burden among Asia countries. For example, there is currently an ongoing initiative with the Asia Pacific Society of Cardiology on heart failure management consensus statement and I am proud to be involved as a representative from the Hong Kong Heart Failure Society in the working group to develop this consensus statement. We also plan to collaborate with cardiology societies in other Asia countries to organise heart failure meetings. Overall, the aim is to increase cross-country collaborations among Asia countries and share the experience and challenges so that we can learn from each other on how to improve heart failure service for our local population.
Q6 What roles would digital tools play in heart failure management from a cardiologist and patient perspective?
Nowadays in the COVID-19 era, the role of telehealth and telemonitoring are increasingly recognized. Some simple but key monitoring parameters such as blood pressure and body weight can be monitored at home and these values can be automatically uploaded to cloud-based server for caring team to review. It would be very useful to monitor any rapid fluctuation in body weight, which may signify fluid retention. The monitoring of blood pressure would be very useful when titrating guideline directed medical therapy or to see any intolerance to heart failure medications. Besides, many cardiac implantable electronic device has remote monitoring function and can be useful to monitor fluid status, activity levels, new arrhythmic events and device malfunction. These data can be monitored by telemonitoring and parent team can be alerted in case of any significant events so that timely intervention can be implemented. With all these digital tools, patients can avoid frequent travelling back to clinic just for the sake of monitoring of these data while the heart failure team can still intervene at appropriate time to prevent heart failure decompensation.